Uterus
Menstrual cycle and the endometrium
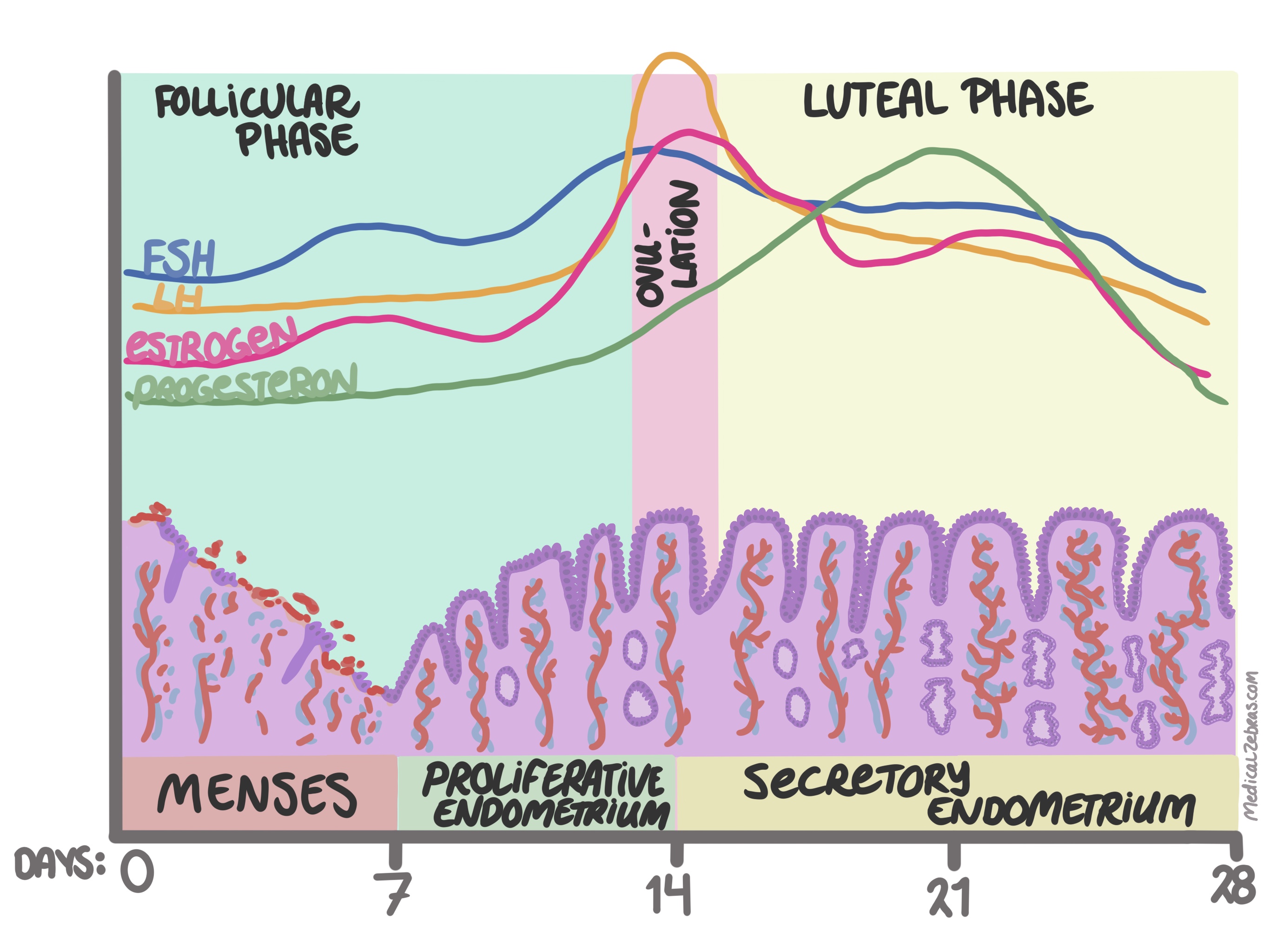
Endometrium
The endometrium is divided into the basalis and functionalis. The basalis is a thin layer of endometrium attached to the underlying myometrium and stays constant over the menstrual cycle. The functionalis lies ontop of the basalis and changes in response to estrogen levels, it sheds during menstration when estrogen levels fall, and grows when estrogen levels increase.Proliferation phase
At the end of menstration the endometrium is lined by a thin basal endometrium and a thin functionalis endometrium. At the start of the proliferative phase, the functional endometrium starts to thicken and there is glandular, stromal and vascular growth. During this time the glands are unifrom and with regular wide space in between them.Histology
- Wide and regular space between glands
-
Glands are uniform
-
Tubular glands, can be mildly dilated
-
The glands are lined with cuboidal or low-columnar epithelium /
cells which is pseudostratified
-
The nuclei is oval to rounded and basally placed. Small nucleoli
might be seen.
-
Mitotic figures are found in the glands
-
Some epithelial cells might be ciliated apically.
-
Stroma is densely cellular
-
Stromal cells are small with oval and hyperchromatic nuclei
-
Cell borders cannot be seen
-
Mitotic figures might be seen (though not as many as in the
glands)
-
A few thin-walled vessel are seen
-
Lymphoid aggrigates might be seen
Secretory phase
During the secretory phase the endometrium continues to thicken and develop. The secretory phase is divided into:-
The early secretory phase (day 16-18)
-
Glands still have a tubular appearance and some mitotic activity.
Subnuclear vacuoles
start to appear, most often first in the midzone of the
functionalis. In the end of this phase, subnuclear vacuoles are
seen in almost all glandular cells. One can assume that ovulation
has occurred if >50% of the glands have at least 50% of the cells
with subnuclear vacuoles.
-
Stroma is identical to late-proliferative phase stroma.
-
The mid-secretory phase (day 19-23)
-
Glandular secreation increases during this phase, seen in the
glandular lumina, and
cytoplasmic vacules move to become supranuclear.
-
Glands become angular
-
Mitotic activity disappears
-
Stromal edema increases, and will be most prominant in the
mid-zone
-
Spiral arteries appear, and stromal cells surrounding them have
eosinophilic cytoplasm. these cells later become predecidual
cells.
-
The late secretory phase (day 24-28)
-
Now glands become
serrated
and tightly packed and predecidual stroma changes are more
evident. Sometimes the precidual cells have a spindle cell
appearance or even signet-ring cell morphology. Lymphocytes are
seen infiltrating the stroma and even neutrophils may be seen.
Menstrual phase
- Endometrial glands are serrated and start to collaps
- Endometrial stroma is compact and starts to collaps into tighty aggregated balls with hyperchromatic nuclei, called "blue balls"
- Other features: Necrotic debris, neutrophils, interstitial hemorrhage, fibrin, apoptotic debris. The glands become tightly packed as the stroma breaks down, even assuming micropapillary morphology (called papillary syncytial metaplasia).
Endometrial polyps
Endometrial polyps are localized overgrowths of endometrial tissue that protrude into the uterine cavity. They can be sessile or pedunculated and vary in size from a few millimeters to several centimeters. They are most commonly found in women aged 40-50 years and are often associated with abnormal uterine bleeding, such as menorrhagia (heavy menstrual bleeding) or metrorrhagia (bleeding between periods). The exact cause of endometrial polyps is not well understood, but they are thought to be related to hormonal imbalances, particularly an excess of estrogen relative to progesterone. Risk factors for developing endometrial polyps include obesity, hypertension, and the use of tamoxifen (a medication used to treat breast cancer). While most endometrial polyps are benign, there is a small risk of malignancy, especially in postmenopausal women. Thus, polyps are often removed and examined histologically to rule out cancer.Histology
-
Glands
-
dilated and irregular, even focal crowding
-
might see epithelial metaplasia
-
often with proliferative activity (even in postmenopausal women)
-
Stroma
-
more fibrous than the normal endometrium
-
collections of thick-walled vessels
-
you might see hyperplastic areas, but they should only be confined
to a few areas of the polyp
Postmenopausal endometrium / Atrophic inactive endometrium
Lack of hormone production from the ovaries, leads to atrophic endometrium as the functionalis layer of the endometrium is no longer stimulated and only a thin layer of basalis endometrium remains. The histological appearance varies, but the endometrium is usually thin with glands that show no proliferative activity. Glands can vary, from being small atrophic tubules (often more prevalent in the immediate years following menopause) and widely spaced to cystically dilated (more often older women), or a combination of both. The glandular cells have small, round to ovoid, dark nuclei and can even be flat in cystic glands. You might see some degree of nuclear pseudostratification, but with no mitotic activity. Though, sometimes, a few mitotic figures can be seen, in women where menopause appears gradually and with uterine prolapse. The surrounding stroma can be densely cellular, but tends to become more fibrous and hypocellular with age. Lymphoid aggregates are often prominent.Disordered proliferative endometrium
Is a benign endometrial change that occurs in response to prolonged estrogen stimulation without the counterbalancing effect of progesterone. This condition is often seen in women with anovulatory cycles, such as those with polycystic ovary syndrome (PCOS) or during perimenopause. In disordered proliferative endometrium, the endometrial glands exhibit irregularities in size, shape, and distribution, leading to a chaotic architectural pattern. The glands may be cystically dilated and show focal crowding and branching. The glandular epithelium typically displays proliferative morphology, but without secretions in the lumen. Tubal metaplasia, characterized by the presence of ciliated cells, is often observed in the glands. The surrounding stroma may show condensation, but lacks the cellular atypia seen in hyperplasia. It is important to distinguish disordered proliferative endometrium from simple endometrial hyperplasia, as the latter carries a risk of progression to endometrial carcinoma. The key differentiating feature is the extent of glandular dilatation; in disordered proliferative endometrium, the dilated glands are focal, whereas in simple hyperplasia, they are more extensive.Histology
- normal to gland stroma ratio is most often normal, but focal glandular crowding and branching may be seen.
- Proliferative morphology but with cystically dilated and irregular glands focally and without secretions in the lumen. These glands often have tubal metaplasia.
- You might see stromal condensation
Endometrial hyperplasia
With unopposed estrogen stimulation there is a risk for endometrial hyperplasia. Endometrial hyperplasia is characterized by an increased gland-to-stroma ratio compared to normal proliferative endometrium. The glands may vary in size and shape, and can be cystically dilated. Based on the architectural complexity and the presence or absence of nuclear atypia, endometrial hyperplasia is classified into three main types:Simple endometrial hyperplasia without atypia Responds well to therapy with progestins (oral pills, injections or with intrauterine device). Has a low risk of progression to endometrial carcinoma.
- Increased gland/stroma ratio
- Glands most often vary in size and shape and cystically dilated
- Only focal crowding of the glands
- Glands are stratified and columnar with light-blue/amphophilic cytoplasm. Nuclei are elongated
- Mitotic activity varies
- Stroma is cellular, more cellular than found in normal proliferative endometrium
- Increased gland/stroma ratio
- Glands can be tubular with or without dilated and more complexed with branching and irreglar outlines
- Glands are more crowded, and even back to back, with little stroma in between
- Glands are stratified, up to four layers
- Mitotic activity varies
- Nuclei are oval and resemble those found in normal glands, mitotic activity can be increased
- Stroma is cellular and cells are spindle in shape as the stroma is compressed between glands
- you might see foamy lipid-laden macrophages
- Nuclear atypia: Cells are stratified with loss of polarity. The nucleus is enlarged, with irregular contours and with coarse or vesicular chromatin. Sometimes with obvious nucleoli
Atypical polypoid adenomyoma
- Glands with variable architectural complexity
- Some nuclear atypia
- Squamous morules is a constant feature
- Glands surrounded by smooth muscle (not cytogenic stroma, like in hyperplasia)
Endometrial metaplasia
Is a response to estrogen or progesteron stimulation. Metaplasia can be diffuse when accompanied by hyperplasia. Metaplasia is often seen in anovulation, polyps, endometritis and trauma.- Papillary Syncytial metaplasia
- Eosinophilic and ciliated cell metaplasia
- Mucinous metaplasia
- Hobnail metaplasia
- Squamous metaplasia
Carcinom in the endometrium
How to identify carcinoma in the endometrium?- Stroma shows desmoplastic reaction => the stroma is more fibrous with spindle shaped cells and elongated nuclei with eosinophilic cytoplasm. However, do not forget that the stroma of a endometrial polyp is often fibrous.
- Glands are confluent and form a complex labyrinth, sometimes even cribiform or forming complex papillary patterns.
- Extensive squamous epithelium with minimal atypia, is only considered a sign of invasion if the stroma around shows desmoplastic reacion
- Intraglandular fibrovascular cores in papillary formation is a sign of papillary hyperplasia, and not cancer.
Gestational trophoblastic disease
Hydatidiform mole
There are two forms of hydatidiform moles depending on the number of chromosomes; complete where the cells are diploid (have 46 chromosomes, all paternal) and partial where the cells are triploid (contain 69 chromosomes; 23 maternal and 46 paternal)Complete hydatidiform mole
-
hydrophic swelling of most villi (edema), from a few mm in diameter
to 3 cm. Some have central cistern formation, a central acellular
space
-
trophoblastic proliferation around the villi with atypia, and
outgrowths of cells (syncytiotrophoblasts and cyncytiotrophoblasts).
This proliferation can be diffuse or only focal
-
usually no fetal tissue
-
the villous stroma has a pale-blue color with widely separated
spindle cells and many blood vessels
-
Implantation site contains intermediate trophoblastic cells that
have more atypical features with higher proliferative activity
Partial hydatidiform mole
-
There is a mixture of two different villi; normal-sized and enlarged
edematous villi occationally with central cisterns (acellular space)
and irregular contours. The small villi often show fibrosis
-
focal trophoblastic hyperplasia is seen, but in lesser extend than
in complete hydatidiform mole, and with minimal atypia
-
invaginations or inclusions in the stroma
-
embryo/fetus may be seen often abnormal features